無菌性髄膜炎について
無菌性髄膜炎は、髄液中に細菌が検出されないにもかかわらず、髄膜(脳と脊髄を包む膜)に炎症が起こる病気です。主な原因はウイルス感染で、発熱、頭痛、悪心・嘔吐、項部硬直(首の硬直)などの症状が現れます12。
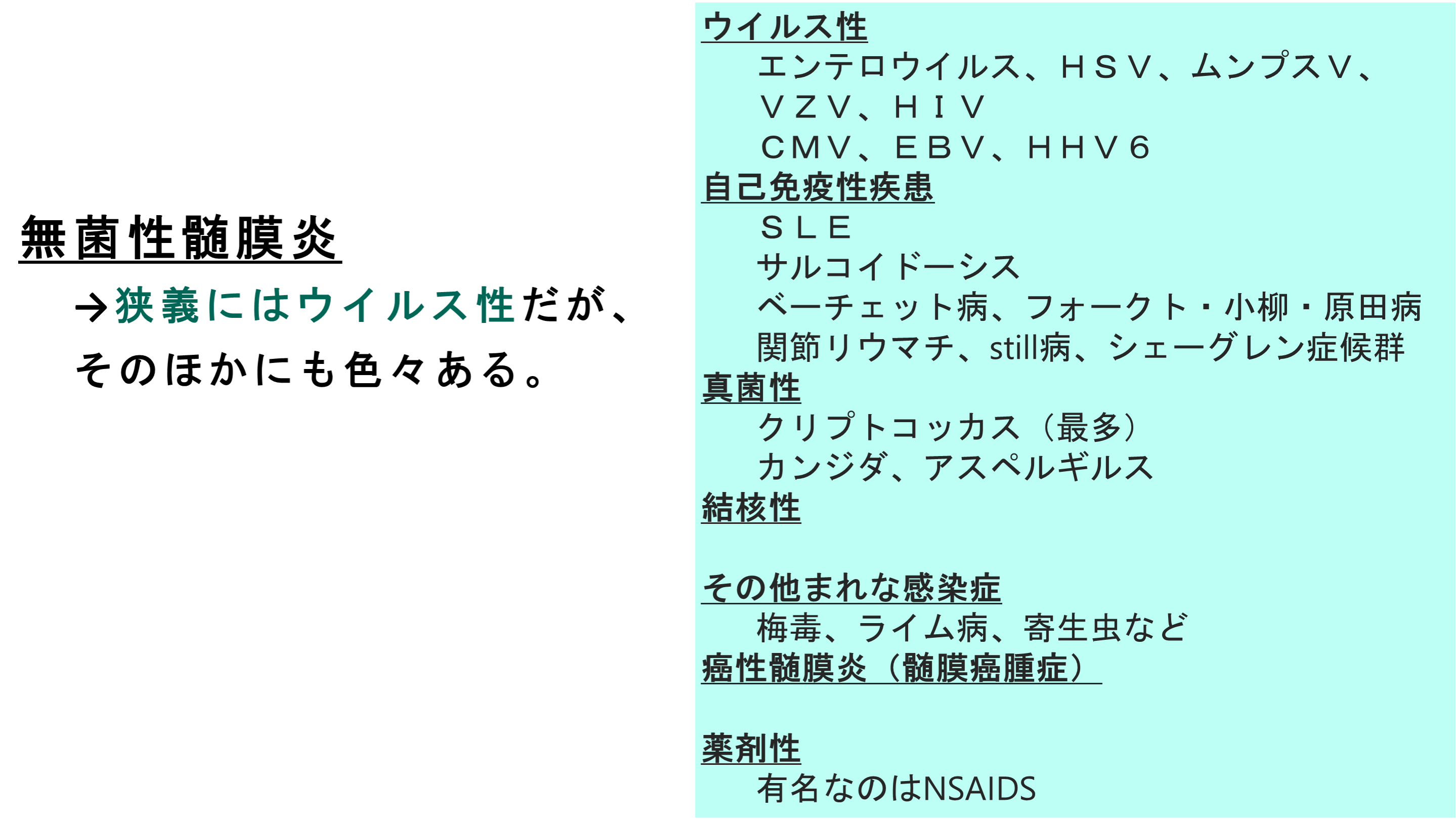
主な原因
症状
- 発熱: 高熱が続くことが多いです。
- 頭痛: 強い頭痛が特徴です。
- 悪心・嘔吐: 吐き気や嘔吐が見られます。
- 項部硬直: 首を前に曲げるのが困難になることがあります12。
診断と治療
診断には髄液検査が用いられ、治療は対症療法が中心です。多くの場合、数日から2週間で回復しますが、重症例では後遺症が残ることもあります12。
Aseptic meningitis is defined as meningeal inflammation - i.e. cerebrospinal fluid (CSF) pleocytosis≥5 cells/mm3 - not related to an infectious process.
Etiologies of aseptic meningitis can be classified in three main groups:
(i) systemic diseases with meningeal involvement, which include sarcoidosis, Behçet's disease, Sjögren's syndrome, systemic lupus erythematosus and granulomatosis with polyangiitis;
(ii) drug-induced aseptic meningitis, mostly reported with non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics (sulfamides, penicillins), intravenous immunoglobulin, and monoclonal antibodies;
(iii) neoplastic meningitis, either related to solid cancer metastasis (breast cancer, lung cancer, melanoma) or malignant hemopathy (lymphoma, leukemia).
Most series in the literature included groups of meningitis that are not stricto sensu aseptic, but should rather be included in the differential diagnosis:
(i) infectious meningitis related to virus, parasites, fungi, or fastidious bacteria that require specific diagnostic investigations;
(ii) bacterial meningitis with sterile CSF due to previous antibiotic administration,
and (iii) parameningeal infections associated with meningeal reaction. Despite progress in microbiological diagnosis (including PCR, and next generation sequencing), and identification of a growing panel of autoimmune or paraneoplastic neurological syndromes, up to two thirds of aseptic meningitis cases are of unknown etiology, finally labeled as 'idiopathic'.
Description of new entities, such as the syndrome of transient headache and neurologic deficits with cerebrospinal fluid lymphocytosis (HaNDL) may decrease the proportion of idiopathic aseptic meningitis. This state-of-the-art review summarizes the characteristics of main causes of aseptic meningitis.
無菌性髄膜炎の治療法は、原因となる病気や炎症の治療に重点を置きます。例えば、無菌性髄膜炎が関節リウマチや全身性エリテマトーデスなどの自己免疫疾患の合併症として現れる場合、まずはその疾患の治療を行います。また、炎症を抑えるためにステロイドや非ステロイド性抗炎症薬が使用されることもあります。
無菌性髄膜炎の予後は、原因となる病気や炎症の進行によって異なります。病気や炎症が適切に管理され、治療が行われることで、無菌性髄膜炎の症状は改善することがあります。しかし、原因となる病気や炎症が進行している場合、予後は悪化する可能性があります。したがって、無菌性髄膜炎の治療には、早期の診断と適切な治療が重要です。
無菌性髄膜炎の注意点と予後については、患者とその家族にとって重要な情報です。医師との定期的なフォローアップや、病気や炎症の管理に努めることが、予後の改善につながるでしょう。
Neurologic involvement in Behçet's disease (BD) is seen in about 5% to 10% of all BD patients. Clinical and imaging data suggest that neurologic involvement in BD presents in two major forms.
The first, central nervous system (CNS) parenchymal involvement with a predilection to brainstem-diencephalic regions, is seen in the majority of patients with neuro-BD (NBD). The second form is cerebral venous sinus thrombosis (CVST), which is seen in up to 20% of cases. BD is very rare in children, but when it does occur, the patterns are reversed: most children with NBD present with CVST. Other syndromes such as spinal cord involvement, arterial CNS involvement, optic neuritis, aseptic meningitis, and peripheral neuropathies may be seen, but are rare. Venous sinus thrombosis in BD has a significantly better neurologic prognosis than parenchymal CNS involvement.
There is no Class I evidence regarding treatment of parenchymal CNS involvement or CVST in BD. Current treatment applications are based largely on expert opinion; none are evidence-based. Acute parenchymal CNS involvement should be treated with high-dose intravenous methylprednisolone (IVMP), 1 g per day, for 5 to 10 days, followed by either a prolonged oral taper or intermittent IVMP pulses with a low oral dose between the pulses, over 6 months. After treatment of the acute attack, long-term maintenance with immunosuppressive agents should be considered in patients with parenchymal CNS involvement, as this form may follow a relapsing or secondary progressive course and may result in significant physical and cognitive deficits leading to severe neurologic disability. A number of randomized controlled studies have tested treatments for systemic manifestations of BD. Colchicine was found to be effective for mucocutaneous symptoms, thalidomide was found to be effective in erythema nodosum-like skin lesions, azathioprine and cyclosporine were shown to be effective in BD uveitis, and cyclophosphamide was shown to be effective for major vascular involvement. More recently, interferon alfa and anti-TNF agents were also shown to be effective in BD uveitis. Although randomized controlled studies have not been performed in NBD, the most widely used long-term therapeutic agent is azathioprine. Recent observations suggest that the addition and long-term use of azathioprine in NBD could be associated with a more favorable course. A growing number of case reports in recent years suggest that anti-TNF agents may be an effective alternative in NBD, but current experience with these agents is limited. CVST in BD is also treated with steroids. The addition to glucocorticoids of anticoagulation, including short-term fractionated heparin, is controversial, as these patients have a higher probability of harboring pulmonary or other aneurysms, which may be associated with an increased risk of bleeding. Long-term oral anticoagulation is unnecessary.
Interestingly, the prognosis of CVST due to BD seems to be much more favorable than the prognosis of CVST due to other causes, with much less tendency for venous infarcts and seizures. However, as recurrences may occur, long-term treatment with azathioprine is recommended.
自己免疫異常による無菌性髄膜炎の報告について、いくつかの事例を紹介します。
非ステロイド性抗炎症薬(NSAIDs)誘発性無菌性髄膜炎:
急性咽頭炎から続発した無菌性髄膜炎:
免疫チェックポイント阻害薬に伴う神経系の免疫関連有害事象:
これらの事例は、自己免疫異常が無菌性髄膜炎の原因となることがあることを示しています。

2024年10月21日 | カテゴリー:頭痛/めまいなど頭部症状, 膠原病, 生活習慣病, 頭頚部症状, 脳神経系疾患, 免疫疾患 |